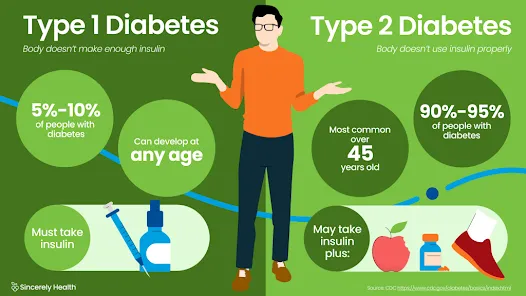
Type 1 diabetes, a chronic autoimmune condition, disrupts the body’s ability to produce insulin—a critical hormone responsible for regulating blood sugar. This condition, once commonly known as juvenile diabetes, can affect individuals of any age, though it most often appears during childhood or adolescence. As an autoimmune disorder, the body mistakenly attacks the insulin-producing beta cells in the pancreas, resulting in a complete lack of insulin over time.
What Is Type 1 Diabetes?
Type 1 diabetes mellitus (T1DM) is an insulin-dependent condition, meaning that daily insulin administration is vital for survival. Unlike Type 2 diabetes, which is often linked to lifestyle and insulin resistance, Type 1 is caused by autoimmune destruction of pancreatic islet cells.
Without insulin, glucose cannot enter the body’s cells and instead accumulates in the bloodstream, leading to hyperglycemia. Over time, high blood sugar levels can damage vital organs and systems, including the heart, kidneys, eyes, and nervous system.
Early Warning Signs and Symptoms of Type 1 Diabetes
Recognizing the early symptoms of Type 1 diabetes can lead to quicker diagnosis and better outcomes. While symptoms may appear suddenly, they often develop over a few weeks.
Key Symptoms Include:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Unintended weight loss despite normal or increased eating
- Extreme hunger (polyphagia)
- Fatigue and weakness
- Blurred vision
- Irritability or mood changes
- Fruity-scented breath, a sign of diabetic ketoacidosis
- Slow-healing sores or frequent infections
In some children, bed-wetting after being dry at night can be an early indicator. If left untreated, Type 1 diabetes can escalate into diabetic ketoacidosis (DKA), a potentially life-threatening complication.
Causes and Risk Factors of Type 1 Diabetes
The exact cause of Type 1 diabetes remains unknown, but a combination of genetic susceptibility and environmental triggers is strongly implicated.
Primary Factors Include:
- Genetics: Specific genes, particularly those in the HLA complex, increase susceptibility.
- Autoimmune reaction: The immune system mistakenly targets and destroys insulin-producing beta cells.
- Environmental triggers: Viral infections, such as Coxsackievirus, rotavirus, or mumps, may initiate the autoimmune response.
- Family history: Having a first-degree relative with Type 1 diabetes increases risk.Geographic patterns: Incidence rates are higher in certain countries, such as Finland and Sweden.
Unlike Type 2 diabetes, diet, lifestyle, or weight are not considered causes of Type 1 diabetes.
How Type 1 Diabetes Is Diagnosed
Timely diagnosis is crucial to prevent complications. Physicians use a combination of blood tests to diagnose and confirm Type 1 diabetes.
Common Diagnostic Tests Include:
- Fasting blood glucose test: High glucose levels after fasting suggest diabetes.
- Random blood sugar test: Elevated glucose levels at any time may indicate the condition.
- Hemoglobin A1c (HbA1c): Reflects average blood sugar levels over the past 2–3 months.
- Autoantibody tests: Detect specific antibodies that attack pancreatic cells.
- C-peptide test: Measures how much insulin the body is producing.
Long-Term Complications of Type 1 Diabetes
Without proper management, Type 1 diabetes can cause significant damage over time.
Chronic Complications Include:
- Cardiovascular disease (heart attack, stroke, hypertension)
- Neuropathy (nerve damage causing pain or numbness)
- Nephropathy (kidney damage leading to failure)
- Retinopathy and vision loss
- Foot ulcers and infections, potentially leading to amputation
- Skin conditions and infections
- Strict glycemic control dramatically reduces the risk of these complications.
Effective Management of Type 1 Diabetes
Living with Type 1 diabetes demands daily attention and care. With the right tools, individuals can maintain healthy lives and reduce risks.
Key Management Strategies:
1. Insulin Therapy
As the pancreas no longer produces insulin, patients require daily insulin injections or insulin pump therapy. Insulin regimens may include:
- Basal insulin: Long-acting to maintain levels between meals
- Bolus insulin: Rapid-acting to cover meals and correct highs
2. Continuous Glucose Monitoring (CGM)
CGM systems track glucose levels throughout the day and night, allowing for real-time adjustments.
3. Carbohydrate Counting and Balanced Nutrition
Meal planning is essential. Patients must learn to:
- Monitor carbohydrate intake
- Balance macronutrients
- Adjust insulin based on meals
4. Physical Activity
Regular exercise improves insulin sensitivity and blood sugar control, but requires careful monitoring to avoid hypoglycemia.
5. Blood Sugar Monitoring
Frequent glucose checks—before meals, after exercise, and during illness—are vital.
6. Education and Support
Ongoing education, diabetes coaching, and support from healthcare providers enhance outcomes.
Living Well With Type 1 Diabetes
With modern technologies and therapies, individuals with Type 1 diabetes lead full, active lives. Key lifestyle considerations include:
- Creating a personalized diabetes care plan
- Maintaining a diabetes emergency kit
- Staying up to date with vaccinations and eye exams
- Collaborating with a multidisciplinary care team: endocrinologists, dietitians, and diabetes educators
Emerging innovations—such as artificial pancreas systems and immunotherapy research—hold promise for even better management in the near future.
Preventive Research and Hope for a Cure
While there's currently no way to prevent Type 1 diabetes, clinical trials are ongoing. Research focuses on:
- Immunotherapy to halt beta cell destruction
- Beta cell regeneration and transplantation
- Genetic therapy
- Artificial pancreas devices that automate insulin delivery
Organizations like JDRF and the ADA continue to fund studies aimed at finding a cure.
Conclusion
Type 1 diabetes is a serious autoimmune condition that requires lifelong management. Early recognition of symptoms, prompt diagnosis, and comprehensive treatment can greatly improve quality of life and minimize complications. With access to proper care, education, and technological advances, individuals living with Type 1 diabetes can achieve exceptional health outcomes and maintain fulfilling, active lifestyles.








0 Comments